These toxins, collectively called endocrine disruptors, are present in nearly every aspect of our environment—not only food, but also personal care products and household goods. Endocrine disruptors are a broad category of chemicals that interfere with the normal functioning of the endocrine system and can create imbalances throughout the body, particularly in the thyroid, reproductive, and adrenal systems. More than 50 different chemicals—found in herbicides, pesticides, fertilizers, plastics, food preservatives, personal care products, meat and dairy, and more—are known to act as endocrine disruptors, says Ann Louise Gittleman, PhD, CNS, author of Before the Change: Taking Charge of Your Perimenopause.
What Are Xenoestrogens?
Xenoestrogens, one of the more troubling types of endocrine disruptors, mimic estrogens and attach to the body's estrogen-receptor sites, in both women and men. These xenoestrogens interfere with hormonal signaling and are believed to cause an increased risk of breast, prostate, and reproductive cancers; reduced fertility; early puberty in children; menstrual irregularities; endometriosis; and other disorders. A new area of research is now pointing to the obesogenic effects of xenoestrogens and other endocrine disruptors: chemicals that disrupt our hormones are also making us fat, says Bruce Blumberg, PhD, professor of developmental and cell biology at the University of California, Irvine.
That's not to say the die is cast. You can't change your past, but you can change your future. Here's how.
Eliminate! A Whole-House Guide to Xenoestrogens
We thought if we kept the Tupperware out of the microwave and used only natural deodorants, we were safe from xenoestrogens. Boy, were we wrong! These toxic compounds are everywhere. Here's your room-by-room rundown for eliminating xenoestrogens, starting with the kitchen:
THE PANTRY. Start with your food shelves. Most processed food contains some kind of undesirable material, says Blumberg, either in the packaging itself or the ingredients. Canned foods are usually packed in cans lined with plastic coating that contains bisphenol-A (BPA), a xenoestrogen. According to an Environmental Working Group (EWG) study, chicken soup, infant formula, and ravioli had BPA levels so high that just one to three servings could expose a woman or child to BPA at levels that caused serious adverse effects in animal tests. Cut back on processed and packaged foods in general, and choose packaged goods in glass or paper containers. Buy grains, nuts, dried fruits, and beans in bulk, and store in glass or stainless steel containers.
THE REFRIGERATOR. Are your milk and burgers organic? If not, they may contain synthetic estrogens, which are used to make cattle grow bigger faster and to increase their milk production. Pesticides on the food the animal eats may also contain xenoestrogens, which can be concentrated in the animal's fat, flesh, and milk. Produce should also be organically grown; anything that's not may contain insecticide or pesticide residues, which can have estrogenic effects, says Blumberg. Buy only organic meat, dairy, and produce, locally whenever possible. If you can't buy all your produce organic, check the EWG's Dirty Dozen list of the most contaminated varieties of fruits and vegetables at foodnews.org and choose low-fat meat and dairy products. HDPE and LDPE (high- and low-density polyethylene) plastics, Nos. 2 and 4 respectively, are hard plastics that are used to make milk jugs and some water bottles. These plastics are generally safe and do not react with the contents of the container.
COOKING AND PLASTICS. You may already know not to heat food in a plastic container, since heating some plastics can cause xenoestrogens to leach out of the container and into the food. But did you know Styrofoam containers contain BPA and that drinking coffee out of a Styrofoam cup causes the BPA to leach out? The moral: never microwave food in anything other than a glass container or on a paper towel. Another source of xenoestrogens comes from Teflon-coated nonstick pans, which if overheated can release endocrine-disrupting perfluoroalkyl compounds, says Blumberg.
FOOD-STORAGE CONTAINERS. Trash your Tupperware and replace it with glass or stainless steel food-storage containers. Or stash food in small glass or metal bowls covered with a saucer. Some plastic cling wrap is made from PVC (polyvinyl chloride), which contains several types of xenoestrogens and other endocrine disruptors, says Blumberg; PVC can leach out, and should never touch food. If possible, buy your (organic) cheese cut to order from the deli, and have it wrapped in plain, uncoated paper; most butcher's paper has a shiny, waterproof PVC coating. Otherwise, shave off any parts that have touched cling wrap, and store the cheese in a glass container or wrapped in paper.
THE KITCHEN SINK. Tap water can contain xenoestrogens from medications and agricultural and chemical pollution. Bottled water isn't always a good solution, since it's usually packaged in flexible plastic that contains phthalates, known endocrine disruptors. Most bottled water is sold in No. 1, (PET or polyethylene terephthalate) plastic containers. However, HDPE and LDPE plastics are safe for drinking water. If you're refilling your hard plastic water bottles at the grocery store, they're probably made of polycarbonate (No. 7), which contains BPA, says Blumberg. Best solution: buy a high-quality activated-carbon water filter, and if you must store your water, use glass bottles.
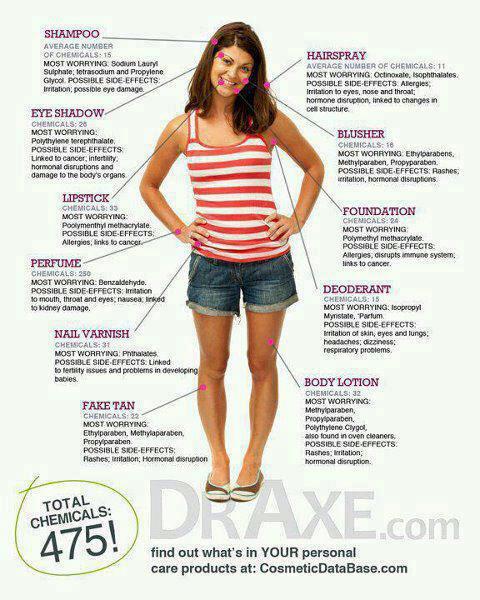
THE BATHROOM CABINETS. Sadly, one of the most effective ways to absorb xenoestrogens is via the skin. Lotions, creams, makeup foundations, nail polish, deodorants, and other personal care products may contain xenoestrogens in the form of parabens, phthalates, and other compounds. Use only personal care products and nail polishes that are clearly marked "paraben free." And if you're using nonoxynol-9 spermicide as your birth control method, find a more natural method; nonoxynol-9 breaks down in the body into xenoestrogenic nonylphenols.
THE BATHROOM SINK. Your toothbrush and bathroom cup are probably made of plastic. As long as you're not eating the toothbrush handle, you're OK. But ditch the cup unless it is No. 2 or 4 plastic, and use a glass or stainless steel one instead. As for toothpaste, it may contain parabens and other xenoestrogens. And the soap or gel you're using to wash your hands and face? You guessed it. Buy chemical-free versions of both.
THE SHOWER. Guess what? Your shower curtain is probably lined with flexible vinyl that contains phthalates, and may contain mercury, dioxins, and lead. Shampoos and conditioners usually contain parabens and other xenoestrogens; a few are made with added estrogen. Use cloth shower curtains or a sliding glass door, and check ingredients on hair care products.
THE BABY'S ROOM. Children are the most sensitive to xenoestrogens and other endocrine disruptors; sadly, any room belonging to children may be filled with xenoestrogens. Baby bottles can be made of rigid No. 7 plastic that contains bisphenol-A. Flexible plastic bottle liners should be made from No. 4 LDPE plastic. Many plastic toys contain phthalates, and flame retardants used in children's clothing are xenoestrogens, says Blumberg. If you do not know what type of plastic it is, don't give it to a child who may put it in her mouth. Consider buying wooden, fabric, paper, and metal games and toys.
THE LAUNDRY ROOM. Dryer sheets are loaded with xenoestrogens that permeate clothing and come into direct, prolonged contact with the skin. Same goes for laundry detergent. Buy only the chemical-free varieties. Skip the dryer sheets altogether, and use natural liquid fabric softener in the rinse cycle. Or try adding 1/2 cup of baking soda to the rinse cycle for softer laundry.
THE BACKYARD. Home lawn care products such as pesticides and weed killers may act as xenoestrogens. In one study, atrazine, a commonly used weed killer, affected animals at doses as small as 0.1 parts per billion. Use the natural versions, or learn to live with weeds.
Fight Back with Nutrition
No matter how diligent you are in removing xenoestrogens from your home, you'll still encounter them in the outside world. Meanwhile, you've certainly been exposed to xenoestrogens sometime in your life. The task, then, is to protect the body from their harmful effects. Certain foods and herbs can shield estrogen receptor sites so xenoestrogens can't attach, help the body metabolize and excrete harmful estrogen, and protect the body from xenoestrogen damage, says Jillian Michaels, a trainer for television's The Biggest Loser and author of Master Your Metabolism. Some of the best:
BROCCOLI, CABBAGE, KALE, BRUSSELS SPROUTS, AND OTHER CRUCIFERS are rich in indole-3-carbinol (I3C), which the body converts to diindolylmethane (DIM), says Shari Lieberman, PhD, CNS. DIM then induces certain enzymes in the liver to block the production of the toxic estrogens and step up the production of the beneficial forms. The best way to eat them is lightly steamed to protect I3C levels or, better yet, pickled: some studies have attributed the low rates of breast cancer in Polish women to their high daily consumption of sauerkraut. Crucifers are also high in sulforaphane, a powerful breast-cancer inhibitor. Best protection: add steamed broccoli to salads; roast cauliflower and Brussels sprouts in olive oil; try sauerkraut or kimchee, a spicy fermented cabbage. Supplements of I3C are available at health food stores; a typical dosage is 150–300 mg per day.
FLAX is the richest source of secoisolariciresinol diglycoside (SDG), a compound that the body converts into lignans, says Michaels. Lignans are phytoestrogens and help balance the body's estrogen levels by binding to the same estrogen receptor sites that xenoestrogens do. When a receptor site is already occupied by a phytoestrogen, xenoestrogens can't attach to it. However, phytoestrogens may not stimulate the receptor causing a lower estrogenic effect. Lignans appear to be especially protective against breast cancer. One study found that women with the highest amount of dietary lignans had a 17 percent lower risk of developing breast cancer. Best protection: sprinkle ground flaxseeds over yogurt, add them to smoothies, stir them into cooked whole grains.
LENTILS are high in soluble fiber, which works as an estrogen-disposal system, says Michaels. Estrogen and xenoestrogens are normally pulled from the bloodstream by the liver and moved to the intestines. In the intestines, fiber soaks up estrogen like a sponge and removes it from the body with other waste. Other foods high in soluble fiber include apples, barley, beans, psyllium, and oat bran. Best protection: eat lentils with curry (it contains extra-protective curcumin), sprinkle oat bran over cereal, serve barley with cooked beans.
 POMEGRANATE can help block estrogenic activity by as much as 80 percent, says Michaels, and help prevent several types of breast cancer cells from multiplying; another study found similar effects on prostate cancer cells. Best protection: add pomegranate juice to green tea, scatter pomegranate seeds over salads, or add them to yogurt. Soy contains phytoestrogens called isoflavones, compounds that mimic estrogen, but in a weaker form. These weaker estrogens then block the receptor sites so xenoestrogens can't attach, says Michaels. They don't accumulate in the body like xenoestrogens, and they're metabolized more quickly.
POMEGRANATE can help block estrogenic activity by as much as 80 percent, says Michaels, and help prevent several types of breast cancer cells from multiplying; another study found similar effects on prostate cancer cells. Best protection: add pomegranate juice to green tea, scatter pomegranate seeds over salads, or add them to yogurt. Soy contains phytoestrogens called isoflavones, compounds that mimic estrogen, but in a weaker form. These weaker estrogens then block the receptor sites so xenoestrogens can't attach, says Michaels. They don't accumulate in the body like xenoestrogens, and they're metabolized more quickly.
SOY is a double-edged sword, however, says Gittleman. Some studies have suggested that high concentrations of soy isoflavones contribute to breast cancer. In addition, soy isoflavones can disrupt normal thyroid hormone function. Eat soy in moderation, avoid concentrated soy products, such as protein powders, bars, and soymilk, and check with your doctor about soy consumption if you're at high risk for prostate, breast, or uterine cancer. Best protection: add edamame to salads, crumble cooked tempeh over brown rice, stir miso into soups.
Excerpt from Sexy Hormones, by Lorna R. Vanderhaeghe, MS
Every woman from the age of menstruation until death should be taking the following nutrients every day to protect her cervix, breasts, ovaries, and uterus, and for menstruating women, to make periods effortless. These nutrients—d-glucarate, green tea extract, curcumin, milk thistle, sulforaphane, chaste tree berry, evening primrose or borage oil, and indole-3-carbinol (discussed above)—do not contain any estrogenic compounds.
D-GLUCARATE is found in all fruits and vegetables, with the highest concentrations found in apples, grapefruit, and broccoli. It is a very important nutrient that helps detoxify excess estrogens and protects from the toxic estrogens made by the liver. This nutrient is especially important if you are taking hormones of any type. Recommended dosage: 150–300 mg per day.
GREEN TEA EXTRACT is a powerful antioxidant containing polyphenols, catechins, and flavonoids, which have been shown to be protective against estrogen-dominant conditions and related cancers, especially breast and ovarian. Green tea extract helps eliminate xenoestrogens and supports the liver in metabolizing fats and hormones. Recommended dosage: 100–200 mg per day (look for products with 60 percent polyphenols) or drink green tea throughout the day. Curcumin is the yellow pigment of turmeric, one of the chief ingredients in curry.
CURCUMIN is a powerful anti-inflammatory, and it also helps eliminate cancer-causing estrogens and environmental estrogens via the liver. Curcumin increases detoxification. Recommended dosage: 50–100 mg per day. Use the spice turmeric in cooking too.
MILK THISTLE, called the protector of the liver, is extremely important for proper estrogen balance in the cells of the body. It detoxifies a wide range of hormones, drugs, and toxins, among other things. Recommended dosage: 50–100 mg per day (ensure that your milk thistle contains at least 80 percent silymarin, an active ingredient in the herb).
SULFORAPHANE from broccoli sprout extract has been shown to stimulate the body's production of detoxification enzymes that eliminate toxic estrogens and balance estrogens in the body. Recommended dosage: 200–400 mcg per day.
VITEX (chaste tree berry), also called the progesterone-enhancing herb, contains no hormones, has no direct hormonal activity, and is not phytoestrogenic. Its main active ingredients work on the pituitary gland to stimulate the production of luteinizing hormone, which in turn increases progesterone and helps regulate the menstrual cycle. It is recommended for irregular or heavy periods, cramps, polycystic ovary syndrome, PMS, breast tenderness, bloating, depression and mood swings, reduction of ovarian cysts, acne related to hormonal imbalance, infertility, endometriosis, and many other female-related symptoms. Recommended dosage: 2–4 capsules per day with food.
EVENING PRIMROSE, BORAGE, andBLACK CURRENT SEED OIL are classified as "good" omega-6 oils and have been shown in clinical studies to be breast-cancer protective. GLA is known to ease cramps and breast pain, and reduce PMS, depression, and bloating. Recommended dosage: 4,000 mg of borage oil or 8,000 mg of evening primrose oil, every day with food.












 About Laura: Laura uses her knowledge of traditional and biologically appropriate diets to improve her clients’ health. Growing up with a family that practices Weston A. Price principles of nutrition, she understands the foods and cooking practices that make up a nutrient dense diet.
About Laura: Laura uses her knowledge of traditional and biologically appropriate diets to improve her clients’ health. Growing up with a family that practices Weston A. Price principles of nutrition, she understands the foods and cooking practices that make up a nutrient dense diet.






