Many of our guests (salon family) are fast paced - multitasking -super women! Naturally, this brings on excess stress, fatigue and hormonal challenges over a period of time.
Common first experiences of hair loss is after giving birth. Years later women reach menopause or other hormonal imbalances, and all not uncommon for women to start losing hair. And while hair loss is a normal process - it’s also something that can be remedied by addressing underlying health and hormonal problems.
I appreciate the recent post shared by Dr. Sara Gottfried MD. You may know of her most recent book "The Hormone Cure." Sara understands the fundamentals of functional medicine and how it relates to women's health and hormones - inside out. Enjoy the quick read and thank you, Sara!

4 Hormone Horrors that Cause Hair Loss
If hormones can zap your energy and steal your sex drive, it’s probably no surprise that they can also turn your tresses into a mess. Here are just a few ways that hormonal issues can cause hair loss:
1. Excess Estrogen.
Estrogen, the power player in women’s bodies, is your friend when it’s appropriately balanced. It makes you feel energized, helps stabilize your moods and contributes to a healthy sex drive. Yet too much estrogen, which can be caused by weight gain, perimenopause or toxicity from exposure to endocrine disruptors (which are rampant in our food, water and plastic products), can lead to thinning hair. During and after pregnancy, for example, estrogen levels peak and then dip, causing sudden hair loss for many women.
2. Insulin Issues.
Insulin, that helper hormone in charge of regulating blood sugar levels, also affects a number of different body processes, including fat storage, heart health and, you guessed it, hair growth. One study published in the European Journal of Cardiovascular Risk found that women with some markers of insulin resistance have a greater risk for androgenic alopecia (AGA), or female pattern baldness.
3. Tricky Testosterone.
In men, testosterone is associated with being big, burly and hairy. But too much testosterone in women creates all sorts of unpleasant results. Namely, it can cause hair growth on the face, neck or chest, and hair loss on your head. Not pretty.
4. Thyroid Woes.
Your body is an intelligent system. So when it’s under stress due to hormonal imbalances, like fluctuating thyroid levels, it redirects energy used for noncritical processes (hair growth) to more important matters at hand (balancing your hormones). Low thyroid is often the cause of that thinning scalp some women get as they age.
3 Ways to Maintain your Mane
If you’re tired of yanking out gobs of hair from the bathroom drain or piling on products to pump up your ponytail, here are three strategies that have helped many of my patients address the root cause of hair loss:
1. Get tested.
Because there are a number of different factors that can contribute to hair loss, it’s best to ask your doctor for a few different tests. I recommend checking: fasting glucose, iron levels and complete blood count (which can determine if you have anemia), as well as thyroid, estrogen and testosterone levels. These assessments should give you a better understanding of what hormonal issues may be at the root of your problem.
2. Eat clean.
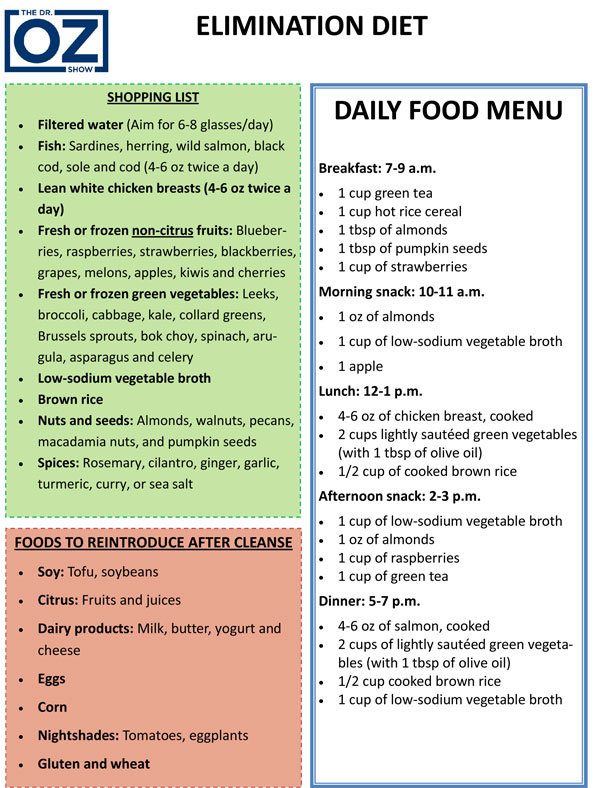
Incorporating more fiber into your diet will help to lower estrogen levels through the process of “elimination” (i.e., excess estrogen will come out in the wash). Focusing on a high-protein,

low-carbohydrate diet with lots of veggies will improve insulin resistance that may be contributing to hair loss.
3. Pop a quality multivitamin.
Nutrients, or lack thereof, can affect hair growth, too. Vitamin A helps fat synthesis in hair follicles, encouraging growth; vitamin E helps protect your hair cells from damage; and B vitamins also help to restore hair thickness and shine. Vitamin C and zinc also help to repair cellular damage from the inside out, which makes for a healthy mane.
Unfortunately, there’s no magic solution, pill or product that will correct hair loss entirely. But if you think of your hormones as a cast of characters, knowing which ones are leading the show and which ones are only playing a supporting role can help you get to the bottom of the issue. Manage your stress levels and get enough sleep. This will help with general hormone balance and can protect your precious locks from any further damage.
Find Sara's article here!